The molecular weight of peptide drugs is between small molecule drugs (<500 Da) and biological products (>5000 Da). The FDA defines peptides as polymers composed of less than 40 amino acids (500-5000 Da). Compared with small molecule drugs and biological products, peptides have many advantages: simpler design, interaction with underexplored targets, cheaper synthetic price, lower immunogenicity, better tissue permeability, deliver drugs to specific targets. So far, more than 100 peptide drugs have been approved for the market to treat a series of diseases.
Last week, Oncopeptides announced that the US FDA has accelerated the approval of its “first-in-class” anti-cancer peptide conjugated drug Pepaxto to be used i combination with dexamethasone for the treatment of relapsed/refractory multiple myeloma (MM) adult patients. The potential of peptide-drug conjugates (PDCs) in targeted therapy has also attracted a lot of attention. This article mainly introduces the basic structure, advantages, and disadvantages of PDC.
A significant limitation of peptides is that they are taken orally, which often destroys their biological activity. Most of the time, they need to be administered intravenously (IV). Compared with biological products, peptides have a shorter circulating half-life, often only a few days to a few weeks, so they need to be administered more frequently.
In addition, most peptides are rapidly cleared by the kidneys in the human body, which makes it difficult to carry out peptide research in vivo. Several methods currently used to improve the druggability of peptides include improving the cell permeability of peptide molecules, enhancing chemical and proteolytic stability, and reducing renal clearance, thereby prolonging the circulatory half-life.
Specifically, methods for improving the enzymatic and chemical stability of polypeptides through chemical modification include:
- Cyclization technology
Cyclization technology has been widely used in the field of peptides, and cyclization has been achieved in a variety of ways: including head to tail, head/tail to side chain, or side chain to side chain;
- Protein modification
The side chain of amino acids provides another good source for protein modification. As the enzyme recognition site is destroyed, the increase in the volume of the side chain will increase its stability;
- Reduce renal clearance through chemical modification;
- Improve the oral bioavailability of peptide therapeutics through formulations, including penetration enhancers and acid-stable coatings.
Faced with the huge unmet clinical needs for cancer treatment, antibody-conjugated drugs (ADC) have received more and more attention. In 2000, Mylotarg (gemtuzumab ozogamicin) became the first ADC drug approved by the FDA, which was composed of an antibody targeting the leukemia cell surface antigen CD33 combined with a cytotoxic payload derived from calicheamicin. In the past 20 years, many ADCs have been approved for the treatment of various cancers. As of September 2020, the FDA has approved a total of 9 ADC drugs. Although ADC continues to improve, there are still several shortcomings:
- First, as cytotoxic drugs, ADCs can cause significant side effects;
- Secondly, the complex structure of ADC leads to high production costs;
- Finally, due to the high molecular weight and protein-like physical and chemical properties of ADC, its efficacy in the treatment of certain types of solid tumors is not ideal.
To overcome these problems, many researchers are exploring the feasibility of peptide-conjugated drugs (PDCs) in targeted cancer therapy.
Structure of PDC
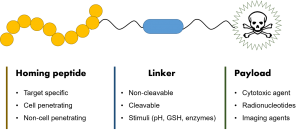
The structure of PDC is similar to that of ADC, and the only difference is the part of the homing device. PDC is composed of three important components: a homing peptide, a linker, and a cytotoxic payload. The payload is delivered by targeting the receptors of tumor cells. Although ADC is developing rapidly, the development of PDC is relatively slow. Currently, there is only one approved therapeutic PDC, 177Lu-dotatate, for the treatment of gastrointestinal pancreatic neuroendocrine tumors (GEP-NETs).
A schematic of a peptide–drug conjugate. Consisting of a homing peptide, a linker, and a payload.
- Homing peptides
Homing peptides can specifically target protein receptors overexpressed on the surface of tumor cells. The secondary structure of the homing peptide has a significant effect on its binding affinity. Most of the homing peptides used so far are linear: although they exhibit good binding properties, they still have several disadvantages, including easy end degradation by enzymes, chemical instability, and rapid clearance by the kidneys. Overcoming these shortcomings can be achieved through methods such as cyclization.
- Linker
According to the required PDC mechanism, different linkers will be used. The linker must maintain stability during delivery to prevent the premature and non-specific release of the drug. Like ADC, the linker used for PDCs can be cleavable or non-cleavable.
- Cytotoxic payload
There are a series of cytotoxic drugs that can be used for cancer treatment, but each drug usually has certain limitations. The biggest limitation is that the drug is non-specific to target cancer cells, which can cause harm to healthy cells and cause serious side effects. The most commonly used payloads in PDC include Doxorubicin, Taxol, Daunorubicin, Gemzar, and Mertansine. PDC can not only be used as a therapeutic drug but also widely used as an imaging agent.
Disadvantages of PDC
Similar to peptides, one of the disadvantages of PDC is its poor circulatory stability and will be quickly cleared by the kidneys. PDC must remain stable in the circulation to prevent the early release of cytotoxic payloads and lead to systemic exposure. There have been studies using different nanoparticles to enhance the stability of PDC.
Another disadvantage of PDC is that the current oral administration efficiency is low, and it needs to be administered by IV injection. Different studies are trying to improve this phenomenon, including different modifications to enhance its chemical and enzymatic stability, and the use of new nanomaterials that deliver peptides and proteins in a controlled manner.
The latest developments in chemistry and biology have expanded our understanding of the advantages and limitations of peptides and laid the foundation for PDC as a new targeted therapy method. We look forward to the advancement of technology, more PDC drugs will come out as soon as possible, benefiting more patients.
References:
- Bethany M. Cooper, Jessica Iegre, Daniel H. O’ Donovan, Maria Ölwegård Halvarsson and David R. Spring. Peptides as a platform for targeted therapeutics for cancer: peptide–drug conjugates (PDCs). Chemical Society Reviews. 2021; 50:1480-1494.