2018-03-02
Insulin was discovered by Banting and Best in 1921. Soon afterwards manufacturing processes were developed to extract the insulin from porcine and bovine pancreas. From 1921 to 1980, efforts were directed at increasing the purity of the insulin and providing different formulations for altering time action for improved glucose control. Purifcation was improved by optimizing extraction and processing conditions and by implementing chromatographic processes (size exclusion, ion exchange, and reversed-phase) to reduce the levels of both general protein impurities and insulin-related proteins such as proinsulin and insulin polymers. Formulation development focused on improving chemical stability by moving from acidic to neutral formulations and by modifying the time-action profle through the use of various levels of zinc and protamine. The evolution of recombinant DNA technology led to the widespread availability of human insulin, which has eliminated issues with sourcing constraints while providing the patient with a natural exogenous source of insulin. Combining the improved purifcation methodologies and recombinant DNA (rDNA) technology, manufacturers of insulin are now able to provide the purest human insulin ever made available, >98 %. Further advances in rDNA technology, coupled with a detailed understanding of the molecular properties of insulin and knowledge of its endogenous secretion profle, enabled the development of insulin analogs with improved pharmacology relative to existing human insulin products.
Chemical Description
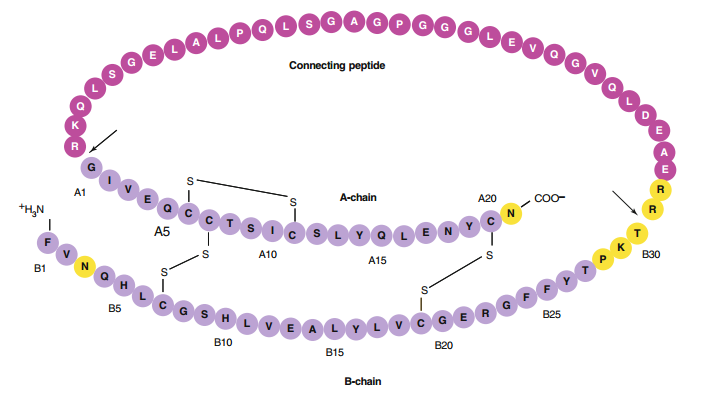
Insulin, a 51-amino acid protein, is a hormone that is synthesized as a proinsulin precursor in the β-cells of the pancreas and is converted to insulin by enzymatic cleavage. The resulting insulin molecule is composed of two polypeptide chains that are connected by two interchain disulfde bonds (Fig. 1). The A-chain is composed of 21 amino acids, and the B-chain is composed of 30 amino acids. The interchain disulfde linkages occur between A7-B7 and A20-B19, respectively. A third intra-chain disulfde bond is located in the A-chain, between residues A6 and A11.
| CAT# | P02018 | I02010 | I02006 |
| Product Name | Insulin B (13-23) | Insulin B (22-25) | Insulin B (9-23) |
| Sequence | EALYLVCGERG | RGFF | SHLVEALYLVCGERG |
| M.W/Mr. | 1209.4 | 525.61 | 1645.9 |
In addition to human insulin and insulin analog products, which are predominately used today as frstline therapies for the treatment of diabetes, bovine and porcine insulin preparations have also been made commercially availabl. However, all major manufacturers of insulin have discontinued production of these products, marking an end to future supply of animal-sourced insulin products. Diffculties obtaining suffcient supplies of bovine or porcine pancreata and recent concerns over transmissible spongiform encephalopathies associated with the use of animal-derived materials are major reasons for the product deletions.
The net charge on the insulin molecule is produced from the ionization potential of four glutamic acid residues, four tyrosine residues, two histidine residues, a lysine residue, and an arginine residue, in conjunction with two α-carboxyl and two α-amino groups. Insulin has an isoelectric point (pI) of 5.3 in the denatured state; thus, the insulin molecule is negatively charged at neutral pH.
In addition to the net charge on insulin, another important intrinsic property of the molecule is its ability to readily associate into dimers and higher-order associated states. The driving force for dimerization appears to be the formation of favorable hydrophobic interactions at the C-terminus of the B-chain. Insulin can associate into discrete hexameric complexes in the presence of various divalent metal ions, such as zinc at 0.33 g-atom/monomer, where each zinc ion (a total of two) is coordinated by a HisB10 residue from three adjacent monomers. Physiologically, insulin is stored as a zinccontaining hexamer in the β-cells of the pancreas. As will be discussed later, the ability to form discrete hexamers in the presence of zinc has been used to develop therapeutically useful formulations of insulin.
Commercial insulin preparations also contain phenolic excipients (e.g., phenol, m-cresol, or methylparaben) as antimicrobial agents. These phenolic species also bind to specifc sites on insulin hexamers, causing a conformational change that increases the chemical stability of insulin in commercial preparations. X-ray crystallographic studies have identifed the location of six phenolic ligand binding sites on the insulin hexamer and the nature of the conformational change induced by the binding of these ligands. The phenolic ligands are stabilized in a binding pocket between monomers of adjacent dimers by hydrogen bonds with the carbonyl oxygen of CysA6 and the amide proton of CysA11 as well as numerous van der Waals contacts. The binding of these ligands stabilizes a conformational change that occurs at the N-terminus of the B-chain in each insulin monomer, shifting the conformational equilibrium of residues B1 to B8 from an extended structure (T state) to an α-helical structure (R state). This conformational change is referred to as the T<−>R transition and is illustrated.
In addition to the presence of zinc and phenolic preservatives, modern insulin formulations may contain an isotonicity agent (glycerol or NaCl) and/or a buffer (e.g., sodium phosphate). The former is used to minimize subcutaneous tissue damage and pain on injection. The latter is present to minimize pH drift in some pH-sensitive formulations.
Pharmacology and formulations
Normal insulin secretion in the nondiabetic person falls into two categories: (1) insulin that is secreted in response to a meal and (2) the background or basal insulin that is continually secreted between meals and during the nighttime hours. The pancreatic response to a meal typically results in peak serum insulin levels of 60-80 μU/mL, whereas basal serum insulin levels fall within the 5-15 μU/mL range. Because of these vastly different insulin demands, considerable effort has been expended to develop insulin formulations that meet the pharmacokinetic (PK) and pharmacodynamic (PD) requirements of each condition. More recently, insulin analogs and insulin analog formulations have been developed to improve PK and PD properties.
Reference:
Crommelin, D. J., Sindelar, R. D., & Meibohm, B. (Eds.). (2013). Pharmaceutical biotechnology: fundamentals and applications. Springer Science & Business Media.