Hexarelin is an engineered growth-hormone-releasing peptide (GHRP), specifically a hexapeptide (His-D-2-methyl-Trp-Ala-Trp-D-Phe-Lys-NH2), that functions via particular receptors in the pituitary and hypothalamus regions to induce growth hormone production in both animals and humans. Similar to other GHRPs, it exhibits considerable prolactin and adrenocorticotropin (ACTH) cortisol-releasing action.
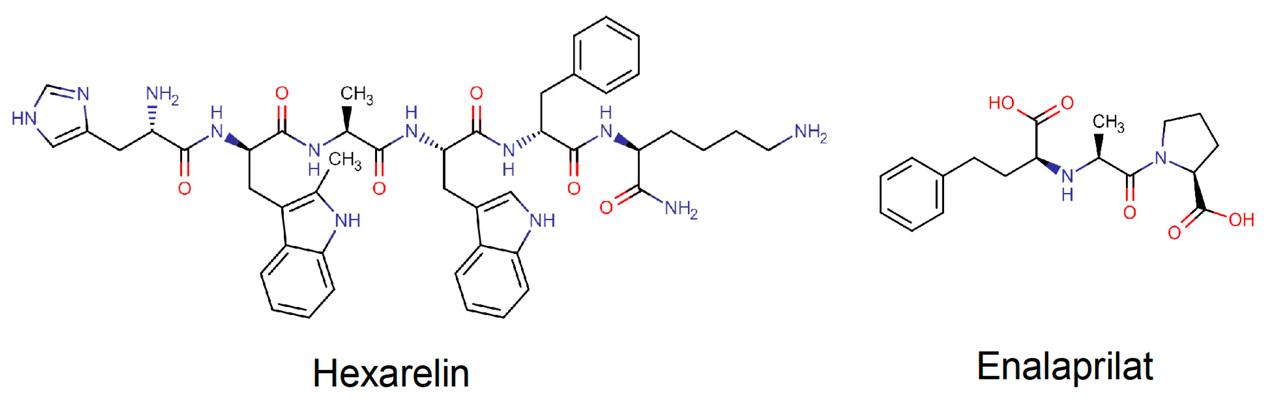 Structures of Hexarelin and Enalaprilat. (Dahlgren D., et al., 2020)
Structures of Hexarelin and Enalaprilat. (Dahlgren D., et al., 2020)
In human, Hexarelin, in single intravenous boluses of 0.5, 1, and 2 ·μg·kg−1, and a placebo, were administered to twelve adult male volunteers. Medications were administered in a rising-dose method, with placebos randomly inserted at periodic intervals, to ensure safety. Following peptide injection, plasma growth hormone concentrations rose dose-dependently, reaching a maximum at 30 minutes after injection and falling to baseline levels within 240 minutes, with a half-life of around 55 minutes.
In dogs, a long terminal half-life of 120 minutes, a fractional plasma clearance of 4.28 ml/min/kg, and a volume of distribution at steady state of 387.7 ml/kg were observed in the pharmacokinetics of hexarelin when administered as an intravenous bolus. Regardless of the increase in dosage provided, the parameters of clearance (3.93-5.17 ml/min/kg) and volume of distribution (316-544 ml/kg) were consistent over the dose range investigated for hexarelin after SC injection.
In rats, volume of distribution at steady state was 744 +/- 81 ml/kg, systemic clearance was 7.6 +/- 0.7 ml/min/kg, and half-life was 75.9 +/- 9.3 minutes after hexarelin was injected intravenously. There was no buildup of hexarelin after s.c. administration, as shown by the area under the curve (477-3826 pmol.min/ml) calculated with increasing dosages. Both the volume of distribution and the clearance/F, which ranged from 1208 to 1222 ml/kg, were independent of dosage. When administered subcutaneously, hexarelin has a bioavailability of 64%. The duodenum, kidney, and liver had the greatest quantities of radioactivity.
An inotropic effect was briefly seen after an acute intravenous injection of hexarelin. Seven healthy male volunteers underwent radioactive angiocardiography to assess their heart function. While hexarelin did not impact mean blood pressure or heart rate, it did enhance left ventricle ejection fraction (LVEF) (70.7 ± 3.0% vs. 64.0 ± 1.5%, P < 0.03). After 15 minutes, LVEF began to rise sharply, reaching a maximum at 30 minutes; the effect continued for up to 60 minutes after administration. Under general anesthesia, 24 male patients with coronary artery disease underwent by-pass surgery. Transoesophageal echocardiography was used to assess LVEF, cardiac output, and cardiac index. Systemic and pulmonary arterial catheterization were employed to determine wedge pressure, central venous pressure, mean arterial pressure, and systemic vascular resistance index. The infusion of hexarelin (2 µg/kg) intravenously caused a quick rise in LVEF, cardiac output, and cardiac index, with a concurrent decrease in wedge pressure. Mean arterial pressure went up and central venous pressure went down momentarily, but neither the heart rate nor the systemic vascular resistance index changed. Additionally, hexarelin induced inotropic effects in rat papillary muscle that were concentration- and time-dependent. It also increased the amplitude of intracellular Ca2+ transients and L-type Ca2+ current, which led to positive inotropic effects in newly isolated adult Wistar rat ventricular myocytes through a protein kinase C signaling cascade.
Hexarelin treatment dramatically reduced angiotensin II-induced apoptosis and DNA fragmentation in newborn rat cardiomyocytes while increasing myocyte viability. Additionally, doxarelin therapy increased the lifespan of H9c2 cardiomyocytes and endothelial cells and prevented doxorubicin-induced apoptosis. Hexarelin's cardioprotective properties may be partly explained by its anti-apoptotic action in cardiomyocytes and endothelial cells. In rats with congestive heart failure, long-term hexarelin treatment reduces LV dysfunction, pathological remodeling, and myocardial cachexia by inhibiting stress-induced neurohormonal activation and cardiomyocyte death.
After 30 minutes of ischemia and 120 minutes of reperfusion, hexarelin (1 µmol/L) significantly decreased the size of infarcts in hearts, according to triphenyltetrazolium chloride staining. However, the protective effect of hexarelin was partially eliminated by the protein kinase C inhibitor chelerythrine. By altering the mitogen-activated protein kinase pathway, hexarelin treatment not only maintains the electrophysiological properties of cardiomyocytes following ischemia-reperfusion injury but also inhibits cardiomyocyte apoptosis, increases cell survival, and has beneficial inotropic effects on ischemic cardiomyocytes. In Zucker rats with low-flow ischemia and reperfusion, ischemic heart damage is reversed by 30 days of hesarelin treatment. Rats given hexarelin showed a far higher degree of left ventricular pressure recovery during reperfusion than controls, although coronary resistance increased just little. In addition to preventing hyperresponsiveness to angiotensin II in the coronary bed of the perfused heart, long-term hexarelin treatment to GH-deficient rats offered significant protection against ischemic and postischemic ventricular dysfunction.
By decreasing interstitial and perivascular myocardial collagen deposition, myocardial hydroxyproline content, and the mRNA and protein expression of collagen I and collagen III, five weeks of hexarelin therapy markedly decreased myocardial fibrosis in spontaneously hypertensive rats. Furthermore, hexarelin therapy reduced the mRNA expression of metalloproteinase-1 inhibitors in cardiac tissue and elevated the activity of matrix metalloproteinases 2 and 9. Furthermore, hexarelin therapy markedly decreased hypertension, left ventricular diastolic dysfunction, and left ventricular hypertrophy. Hexarelin (0.1 µmol/L) treatment of cultured cardiac fibroblasts decreased angiotensin II-mediated elevation of Tgf-β expression and release, slowed collagen synthesis and proliferation, and inhibited transforming growth factor (TGF)-β-induced DNA synthesis.
Hexarelin was shown to have antiatherogenic properties in adult Sprague-Dawley rats. Hexarelin treatment raised serum nitric oxide levels and the mRNA expression of endothelial nitric oxide synthase, GHSR, and CD36 in the aorta of atherosclerotic rats, inhibited the development of atherosclerotic plaques and neointima, and partially reversed the ratio of serum high-density lipoprotein cholesterol to low-density lipoprotein cholesterol. Hexarelin treatment significantly decreased calcium deposition in the aorta wall, foam cell formation brought on by oxidized LDL, and the incorporation of tritiated thymidine in cultured vascular smooth muscle cells. Furthermore, hexarelin administration for an extended period of time dramatically decreased plasma cholesterol concentrations in obese rats while having no effect on the elevated triglyceride levels.
There is a clear structural difference between the synthetic peptides hexarelin and ipamorelin. Ipamorelin is a pentapeptide with five amino acids (Aib-His-D-2-Nal-D-Phe-Lys-NH2), in contrast to hexarelin, which is a hexapeptide with six. These structural differences affect how they attach to and select for the growth hormone secretagogue receptor (GHSR), which in turn affects how much growth hormone they secrete. Hexarelin is ideal for those who want the highest level of hormonal stimulation due to its potent GH-releasing capabilities. Its increased effectiveness, however, sometimes comes with a rise in adverse effects, such as raised levels of prolactin and cortisol. As an alternative, ipamorelin is preferred because to its reduced adverse effects and selective GH release. It is a safer option for long-term use since it does not substantially increase levels of cortisol or prolactin. Therefore, the choice between Hexarelin and Ipamorelin is mostly dependent on the needs and tolerance levels of the individual.
Because of its selectivity, ipamorelin may trigger the pituitary gland to secrete growth hormone without triggering appetite suppression or elevating cortisol levels, neither of which might impair memory development. However, hexarelin has shown to have important neuroprotective properties that help keep cognitive functions, especially memory, intact. The effects of Hexarelin and Ipamorelin on bone health are similar. The skeletal system is improved by hexarelin because of its effectiveness in boosting bone mineral density. At the same time, Ipamorelin, a growth hormone secretagogue, may enhance bone health by promoting the body's natural synthesis of growth hormone. Ipamorelin is a more balanced alternative to Hexarelin as it does not lead to an increase in appetite or excessive production of growth hormone. This is not meant to suggest a clear winner, but rather to highlight the many ways in which different substances contribute to bone health.
Hexarelin and Ipamorelin both have a laundry list of possible negative effects. An increase in appetite, swelling, and tingling or numbness in the limbs are all possible side effects of hexarelin. Cortisol and prolactin levels may also rise with prolonged use. In contrast, ipamorelin is associated with less severe side effects, such as reduced frequency of increased appetite or edema. Still, users run the risk of experiencing side effects such as vertigo, migraines, and, very rarely, injection site reactions. It is crucial to talk to a doctor before starting a new course of supplements, as is the case with any supplement program.
In 2010, the synthetic version of growth-hormone-releasing hormone (GHRH) known as tesamorelin was licensed for the treatment of HIV-associated lipodystrophy. Adding a trans-3-hexenoic acid group to a synthetic peptide that has all 44 amino acids of human GHRH is what makes the medicine what it is. The 44-amino acid sequence of human GHRH is the basis for the N-terminally modified molecule known as tesamorelin. The original peptide is weaker and less stable than this synthetically altered version. Additionally, dipeptidyl aminopeptidase is unable to cleave it as easily as it does human GHRH. It raises insulin-like growth factor (IGF-1) levels and promotes the production and secretion of endogenous GH. In order to control the body's composition, the secreted GH attaches to certain organ receptors. The integration of anabolic and lipolytic pathways is primarily responsible for this control. But research shows that lipolysis and a subsequent drop in triglyceride levels are the primary ways by which Tesamorelin lowers body fat mass.
The N-terminally modified molecule based on the 44 amino acid sequence of human GHRH, Tesamorelin, has a significantly more complicated structure than Hexarelin. The original peptide is weaker and less stable than this synthetically altered version. Additionally, dipeptidyl aminopeptidase is unable to cleave it as easily as it does human GHRH. It raises insulin-like growth factor (IGF-1) levels and promotes the production and secretion of endogenous GH. In order to control the body's composition, the secreted GH attaches to certain organ receptors. The integration of anabolic and lipolytic pathways is primarily responsible for this control. But it has been shown that lipolysis and the consequent decrease in triglyceride levels are the main ways in which Tesamorelin reduces body fat mass, which is not quite the same mechanism of action as Hexarelin.
Used as a diagnostic tool to evaluate growth hormone (GH) production, sermorelin, often known as GHRH (1-29), is a peptide analogue of GHRH. Growth hormone insufficiency is therefore diagnosed with this agent. Thought to be the smallest totally functioning piece of GHRH, this 29-amino acid polypeptide reflects the 1–29 fragment from natural human GHRH. Children suffering with growth hormone shortage or development failure were treated with Sermorelin, which stimulates the pituitary gland to produce GH, hence raising plasma GH levels. Hexarelin, which functions as a GH secretor and stimulates GH secretor receptors in the brain and peripheral tissues, has a different method of action than Sermorelin. Through certain receptors connected to the pituitary gland, Sermorelin mimics physiological processes in the human body. Common adverse effects of both medications include headaches, dizziness, flushing, and injection site reactions. Increased hunger, water retention, and sporadic tingling in the extremities are possible side effects of hexarelin. Muscle atrophy brought on by Sermorelin may result in exhaustion, excessive growth hormone, and metabolic and cardiovascular issues. Hexarelin preserves skin suppleness and boosts bone mineral density. Both peptides are often given via injection, with the most common method being subcutaneous injection.
A synthetic analogue of human GHRH, CJC-1295 is more resistant to proteolytic inactivation by dipeptidyl peptidase IV (DPP-IV) due to the substitution of four amino acids. This major medicinal component is associated with a drug affinity complex (DAC), which permits the CJC-1295 to conjugate with endogenous albumin upon injection, prolonging its half-life to a comparable duration to albumin's. With a single injection, in human subjects, CJC-1295 may increase plasma GH levels by 2- to 10-fold for 6 days or longer and plasma IGF-1 levels by 0.5- to 3-fold for 9 to 11 days. With the inclusion of the DAC additive, the drug has an estimated half-life of about 6 to 8 days in humans. With multiple doses of CJC-1295, IGF-1 levels were found to remain elevated in humans for up to 28 days. Although both CJC-1295 and Hexarelin are growth hormone-releasing peptides, the latter is more potent in stimulating the release of growth hormone.
Unlike the peptide Hexarelin, MK677 is a non-peptide substance with a highly effective and long-lasting oral active ghrelin receptor agonist and growth hormone secretagogue that mimics the GH stimulating effects of the endogenous hormone ghrelin. Studies have shown that it can increase the secretion of several hormones, including growth hormone and IGF-1, and keep plasma levels of these hormones elevated, while also raising cortisol levels. Due to its ability to reverse diet-induced nitrogen depletion, MK-677 shows promise as a treatment for catabolic situations in individuals with specific acute or chronic diseases, provided that these short-term anabolic benefits are sustained.
The GH secretagogue (GHS) family includes the synthetic hexapeptides hexarelin (HEX) and GHRP-2 (D-Ala-d-βNal-Ala-Trp-d-Phe-Lys-NH2), which are superanalogs of GHRP-6. In order to induce GH release, GHS act via particular receptors at the pituitary and hypothalamus levels in both animals and humans. One study compared the GH, PRL, ACTH, and cortisol responses in 6 healthy young people (22-27 years old) to those after 1 and 2 μg/kg IV GHRP-2 and HEX, as well as after 1 μg/kg IV GHRH and 400 μg IV TRH + 2 μg/kg IV hCRH. Also examined were the GH responses to 2 μg/kg IV GHRP-2 or HEX, in comparison to those to 1 μg/kg GHRH, in six healthy senior individuals ranging in age from 66 to 73 years. The GH response in young adults was comparable to that of GHRH and was stronger when given 1 μg/kg IV GHRP-2 and HEX, with the difference being a greater response (p < 0.05). A comparable GH response was induced by the injection of 2.0 μg/kg IV GHRP-2 and HEX, which was greater (p < 0.05) than that after the 1.0 μg/kg dosage. When administered 2.0 μg/kg IV GHRP-2 and HEX to old adults, the GH responses were comparable to and greater than those in young people, but lower (p < 0.01) than those in GHRH (p < 0.05). When compared to TRH, the PRL responses in young adults to all GHRP-2 or HEX dosages were comparable and significantly lower (p < 0.01). Conversely, ACTH and cortisol were equally increased by all GHRP-2 and HEX dosages. The reactions to hCRH were comparable. Ultimately, our findings show that GHRP-2 and HEX both stimulate somatotrope secretion in humans, although to a lesser extent than GHRH; this impact varies with dosage and age. Due to their shared effects on PRL, ACTH, and cortisol levels, GHRP-2 and HEX do not exert completely selective actions. When compared to TRH, GHRPs have a lesser PRL-releasing activity, but they are comparable to hCRH in terms of ACTH/cortisol-releasing activity.
Temporary ligation of the left descending coronary artery (tLAD) was used to produce myocardial ischemia in C57BL/6 J mice. After that, the mice were administered either hexarelin (0.3 mg/kg/day; n = 20) or vehicle (n = 18) for 21 days, with the first dosage given just before reperfusion. Mice with IR damage and sham operations underwent high-field magnetic resonance imaging to evaluate left ventricular (LV) function. Mice treated with hexarelin had considerably better LV function than mice treated with VEH. Significant reductions in interstitial collagen, TGF-β1 expression, and myofibroblast differentiation were seen in the hexarelin-treated animals after 21 days. The results of this study indicate that hexarelin has an anti-inflammatory impact on the myocardium, as the ANS balance shifted to favor the parasympathetic nervous system and cardiac troponin-i and TNF-α levels were significantly reduced.
Research was conducted on adult male rats that had either intact or osteopenic gonadectomy (GDX) to determine the effects of 30 days of therapy with the very strong GH-releasing chemical hexarelin (50 μg/kg, subcutaneous injection twice daily) on bone metabolism and bone mineral density (BMD). Before therapy and at 7, 14, and 30 days following treatment, serum total alkaline phosphatase (ALP), lysyl pyridinoline (LP), and hydroxylysyl pyridinoline (HP) were assessed as indicators of bone absorption. The lumbar spine, femoral shaft, and shaft bone mineral density (BMD) were assessed by dual-energy X-ray absorption both before and after the experiment. On day 7, hexarelin substantially decreased LP (-36.3%) and HP (-22.8%) excretion in intact rats (P<0.05), but it had no effect on serum ALP activity or bone mineral density (BMD). The use of hexarelin entirely averted notable (P <0.01) spikes in androgen deficiency-related increases in urine LP (+143.8%) and HP (+119.4%) excretion, as well as early declines in ALP activity (-26.5%), in the femoral diaphysis (-7.9%) and lumbar spine (-6.8%). A substantial drop (P <0.05) was seen in BMD. Chronically treated rats maintained GH responses following acute stimulation with hexarelin, suggesting that the GH-releasing action of hexarelin is at least largely responsible for its bone protective effect. The fact that hexarelin blocks bone resorption, in contrast to GH, implies that different processes are involved in hexarelin's ability to preserve bone.
Apoptosis, tubular dilatation, high blood creatinine levels, tubular necrosis, and significant kidney injury are the symptoms seen in rats who had ischemia/reperfusion (I/R). Nevertheless, hexarelin preconditioning had protective benefits, reducing renal pathological alterations after ischemia, enhancing renal function, and discouraging cell death. To do this, one study upregulates the anti-apoptotic protein Bcl-2 and downregulate traditional genes associated with cell death, namely Caspase-3, Bax, and Bad. Hexarelin decreased apoptosis in HK-2 cells after I/R, which is in line with in vivo findings. Also, the GSEA analysis demonstrates that the apoptotic pathway is critical for I/R-induced acute kidney injury (AKI). According to molecular docking, Hexarelin has a high binding affinity for MDM2, a well-known negative regulator of the apoptosis-associated protein p53. This suggests that Hexarelin's anti-apoptotic activity is mediated in part by its interaction with MDM2. In vivo and in vitro investigations showed that Hexarelin significantly inhibites MDM2 and p53, lending credence to these results.
Related Peptides at Creative Peptides
FAQ
Is hexarelin a Ghrp-6?
As GHRP-6, hexarelin is a synthetic GHS. Hexarelin is superior to GHRH and GHRP-6 in stimulating GH release. The influence of hexarelin on sleep-endocrine activity and the immune system is unknown.
References